Reduce your blood pressure, increase your longevity

When is the last time you took your blood pressure?
I’ll be honest, blood pressure is not something I measure very often. It hasn’t been an issue in the past for me, so I guess I’ve declared I’M FINE, leave me alone doctors.
Not measuring my blood pressure just creates a blind spot though and isn’t a very proactive strategy. Guilty.
The evidence on blood pressure is clear: optimizing your blood pressure is, other than quitting smoking, the most important modifiable variable in the prevention of major adverse cardiovascular events (MACE).
Since death due to cardiovascular disease is our leading cause of death it’s impossible to underscore the value of monitoring blood pressure for those of us interested in improving our healthspan and lifespan.
What do the numbers mean? What is ‘normal’?
The American Heart Association categorizes the ranges for normal, elevated, Hypertension Stage 1, Hypertension Stage 2 and Crisis as follows:
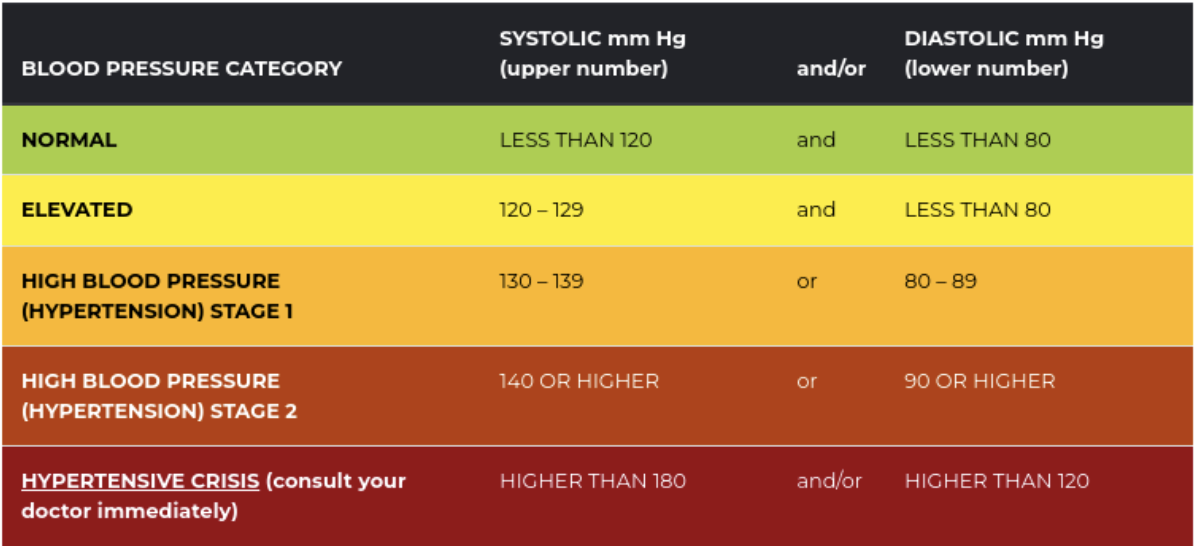
This is a good starting point to understand your measurements. And certainly the increasing urgency in the colour coding helps to illustrate the levels of importance with each increase in blood pressure levels. But should we care if we have a systolic measurement of 125, 130 or 135? Or a diastolic blood pressure reading of 85? What is the risk? And does that target range and risk change with age?
Blood Pressure and Cardiovascular Risk
A large meta analysis published in 2002 with data taken from 61 prospective observational studies involving one million adults with no previous vascular disease showed an almost linear reduction in stroke risk and ischemic heart disease with lower systolic and diastolic blood pressure. This decreased risk with decreased blood pressure was apparent in each decade age 40 to age 80.
Take a quick peek at the key figures from this meta-analysis, Figure 2 looking at stroke mortality risk and Figure 4 Ischemic Heart disease mortality risk.
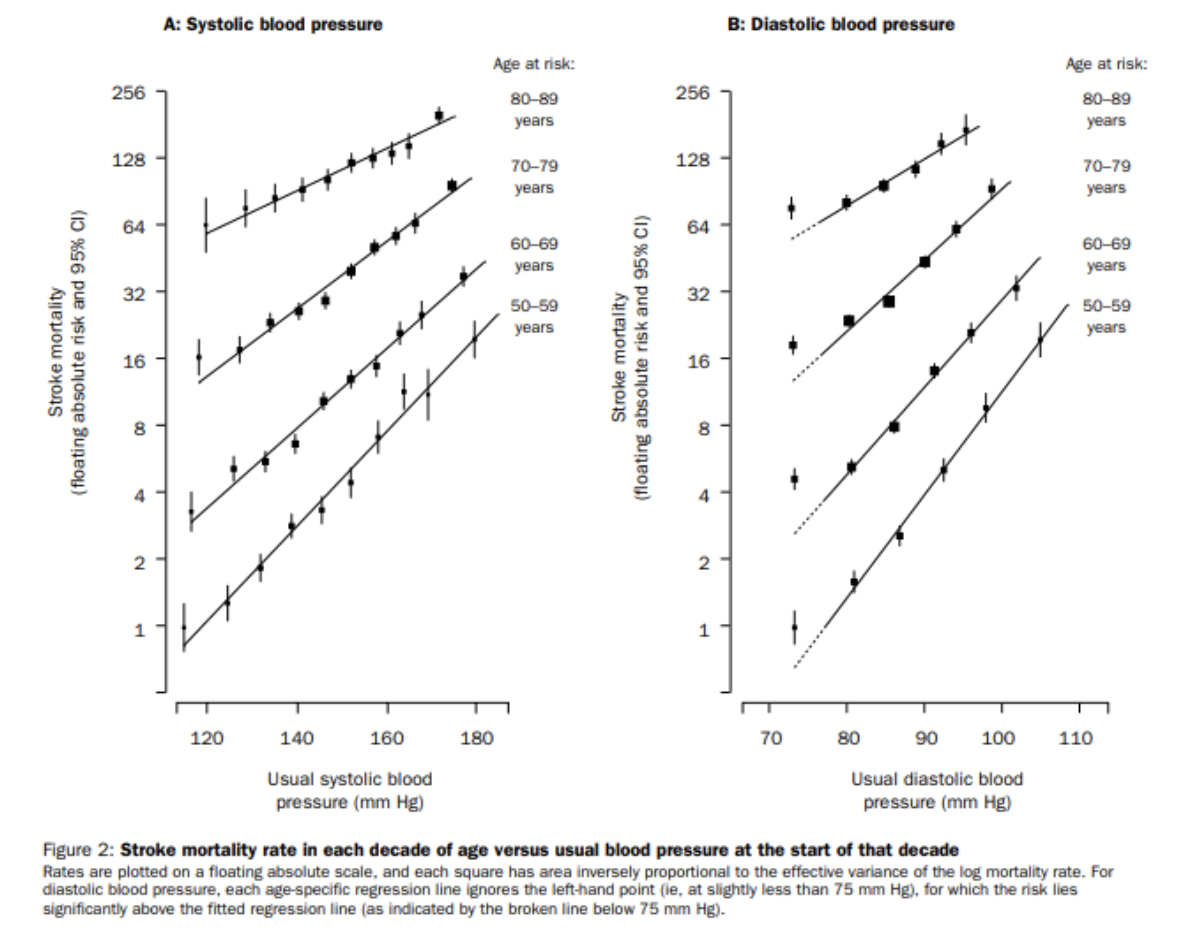
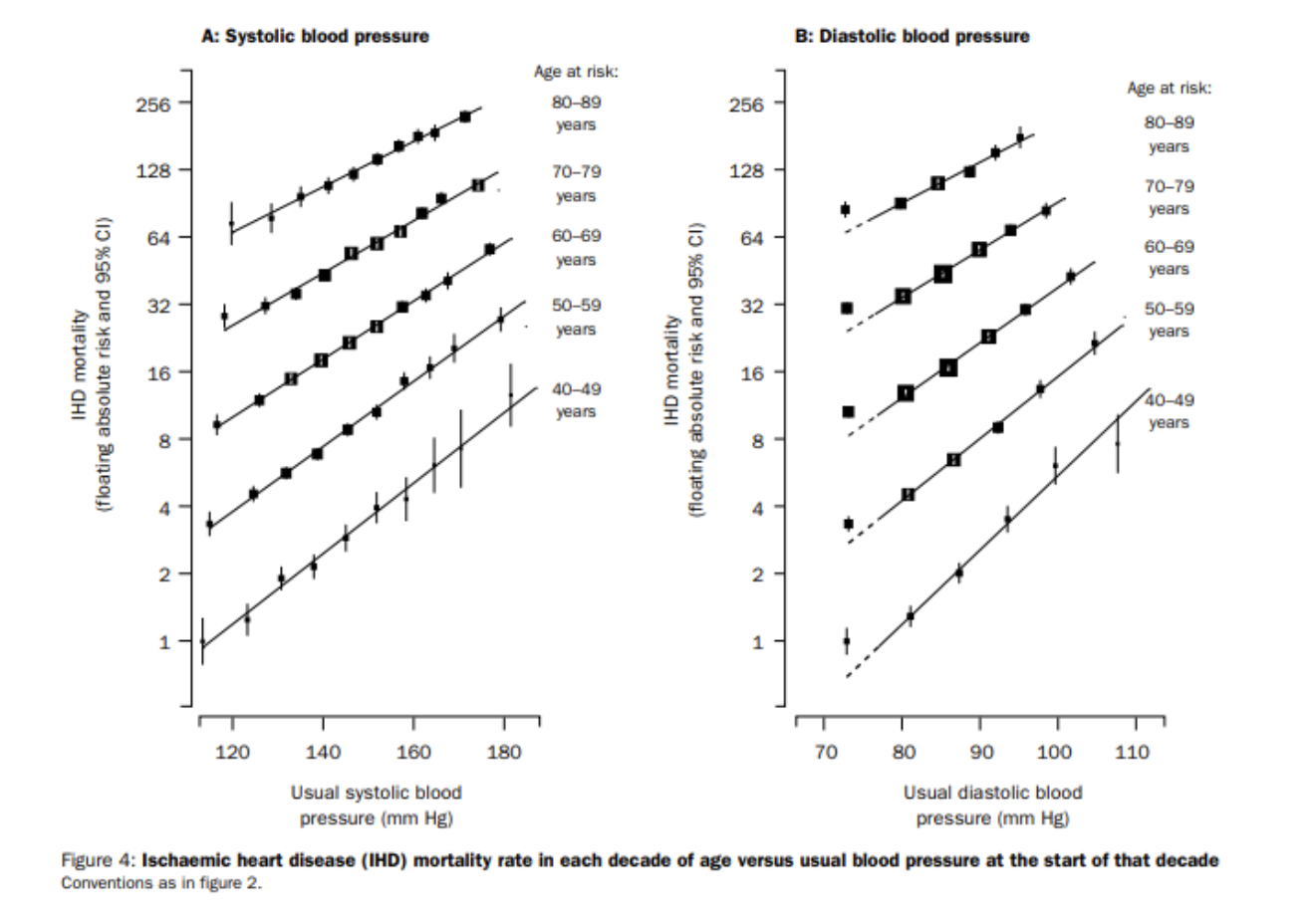 From this data, it appears there is a continuous relationship with risk down to at least as far as 115/75 mm Hg.
From this data, it appears there is a continuous relationship with risk down to at least as far as 115/75 mm Hg.
The authors calculated that a reduction of only 2 mm Hg in systolic blood pressure decreases mortality from cerebral vascular accidents by 10% and cardiovascular disease by 7% in the 5th decade (slightly smallar reductions in older age groups).
The association looks compelling. However, observational based research trials have their pitfalls and correlation in observational research cannot infer causation (as there are often many other variables that could account for the result).
Fast forward a decade or so. A landmark clinical trial funded by the US government dubbed the SPRINT trial published in 2015, has been widely referenced as the best clinical evidence to date to support aggressive management of hypertension. This large randomized controlled trial compared a target threshold goal of <120mm Hg (intensive treatment) with pharmacological therapy versus a target threshold goal of <140mm Hg (standard treatment) with pharmacological therapy in 9361 hypertensive patients (systolic blood pressure 130-180mg Hg) 50 years of age or older.
The classes of blood pressure medications utilized were ACE inhibitor, angiotension receptor blockers or calcium channel blockers.
The trial was cut short at approximately a median follow up of 3.26 years as the results of the primary question being asked were obvious: aggressive management significantly reduces major acute cardiac events (25% reduction in intensive treatment group vs standard treatment) and all cause mortality (27% reduction in the intensive treatment group vs standard treatment).
Researchers concluded that higher medication doses (despite higher side effect profiles) is warranted to widely recommend more aggressive management of blood pressure.
The take home message from these large trials:
-lowering your blood pressure towards 115/75 mm Hg will reduce your risk of acute cardiace events at any age 40+ (but presumably younger as well)
-more aggressive pharmacological treatment targeting <120mm Hg systolic blood pressure results in significant reduction in MACE and all cause mortality
The lower the better. But not too low that you faint, fall and bash your head: blood pressure that is too low can have it’s consequences as well. Although the ‘normal level’ is described as under 120/80mm Hg, many experts state there is no additional benefit to maintaining blood pressure below that threshold.
So as low as possible, without any short term consequences on function.
Exercise to manage blood pressure
What about managing blood pressure without pharmaceutical intervention. The strong results from the SPRINT trial showing aggressive pharmaceutical management resulted in significant reductions in cardiovascular risk. But can we get that similar result from exercise, avoiding the potential side effect of the meds and getting all the other associated benefits of a good exercise program?
The American College of Sports Medicine recommends for individuals with hypertension individuals should exercise on most and preferably every day of the week with an accumulation of 90 minutes to 150 minutes per week. This may be accomplished through a combination of aerobic and resistance exercise.
This is similar to our Canadian physical activity guidelines where adults 18-64 are recommended to get at least 150 minutes of moderate to vigorous aerobic physical activity and resistance training twice a week.
Can we do better than these generic guidelines if we want to get more aggressive with an exercise based approach to reduce and manage blood pressure?
A narrative reveiw of 27 RCT’s published in the British Journal of Sports Medicine in 2016 found that medium to high intensity aerobic exercise done 2-3x/week for 40-60 mins resulted in a mean reduction of 11/5mm Hg after a range of 12-16 weeks on average.
Isometric (or static) physical training showed some similar promise using studies training handgrip isometric strength, 30% max for 2 mins repeated for 4 sets, 3x/week after 8-10 weeks.
Examples of common isometric (static) exercises include a wall sit, a plank or a dead hang. These types of exercises show some promise for blood pressure reduction, however there is limited evidence to date (4 studies) and it is likely too premature to be recommending isometric exercises as a stand alone first line exercise approach. Isometric exercises may be a good alternative primary approach if other forms of exercise aren’t possible.
Some experts such as Peter Attia recommend 3-4 hours of zone 2 aerobic cardiovascular exercise per week. There is likely not a (cardiovascular) upper limit to this zone 2 approach, but I would argue if you are devoting more than 3-4 hours a week to your training you should also incorporate 2 whole body strength training sessions a week (for lean muscles mass growth/maintenance) to round out your blood pressure focused strength and conditioning plan.
What about interval training? A study published in 2010 tested both continuous and interval exercise training in a 16 week program with two 40 minute sessions per week. Workload between the interval training group and continuous training group was the same: 40 mins of 60% peak heart rate for continuous treadmill group and alternating intervals of 50% and 80% peak heart rate for an average of 60% peak heart rate. Both forms of exercise were equally beneficial for blood pressure control, but only interval training reduced arterial stiffness in treated hypertensive subjects.
Incorporating interval training into your blood pressure reduction plan appears to offer some additional benefits to your cardiovascular system that continuous aerobic training doesn’t; so, be sure to add in at least one interval based training session a week. High interval training or sprint training, can be a great time efficient training tool for fat loss and cardiovascular health
Consistency matters for blood pressure measurement
For your blood pressure measurements to have any value in tracking you must have a consistent measurement process. Rushing into your doctors office and quickly taking your blood pressure is known to drastically overestimate your average ambulatory blood pressure.
For consistent measurement you should measure with the same device over an extended period. That includes the same automated cuff or same individual taking your blood pressure with a sphygnomater and inflatable cuff.
Also you need to rest in a seated position prior to testing. My local shoppers drug mart automated cuff directs me to stay seated for one minute prior to testing. In the SPRINT trial discussed above they wait 5 minutes in between each measurement using an automated cuff in a dark room. We recommend stay seated, with focus on quieting your mind and body with some slow deep breathing for 3-4 minutes prior to testing. Be consistent with your testing process.
If you haven’t tested in a while and want to get an accurate starting point before implementing a treatment strategy try measuring in the morning and afternoon for 7 days straight and take an average of those results.
The future of blood pressure monitoring
Current research on continuous blood pressure monitoring uses a cuff that inflates periodically to measure blood pressure throughout the day.
But what if continuous blood pressure was as simple as checking your fitbit, garmin or other fitness and health tracking device on your wrist? The accuracy of cuffless wrist blood pressure measurement is improving and will likely be incorporated in your favorite fitness wearables soon.
This a huge advance for better understanding your blood pressure. For example what happens to my blood pressure during certain physiological stressors. And maybe more important what happens to my blood pressure during my work, commute or home time.
Blood pressure will become the most important piece of data you track on your fitness device for your health and longevity!
